
Frailty is defined as a clinically recognisable state of increased vulnerability resulting from ageing-associated decline in reserve and function across multiple physiologic systems, such that the ability to cope with everyday or acute stressors is compromised.
Components of frailty include: low grip strength, low energy, slowed waking speed, low physical activity, and unintentional weight loss.
Frailty is a common clinical syndrome in older adults that carries an increased risk of poor health outcomes including falls, incident disability, hospitalisation, and mortality. Investigating and managing its causes and progression is important in identifying and developing new approaches for frailty prevention and treatment.

Visual impairment can directly cause problems with mobility and with activities of daily living (ADLs), and low vision has considerable impact on quality of life (QoL), independence, mobility, ability to care for oneself, and risk of falls.
Standard home, work and communal environments often do not actively cater to this segment of society, and there is a need for technology, support and facilities to address the functional mobility needs of the visually impaired.
Visual impairment is a prevalent problem in society, and it has been estimated that 50 million people worldwide have low vision, and a further 18 million are blind, with close to two-thirds of them from the Asia-Pacific region. There is thus a substantial need for programmes to alleviate the difficulties in mobility and physical function encountered by individuals with visual impairment.
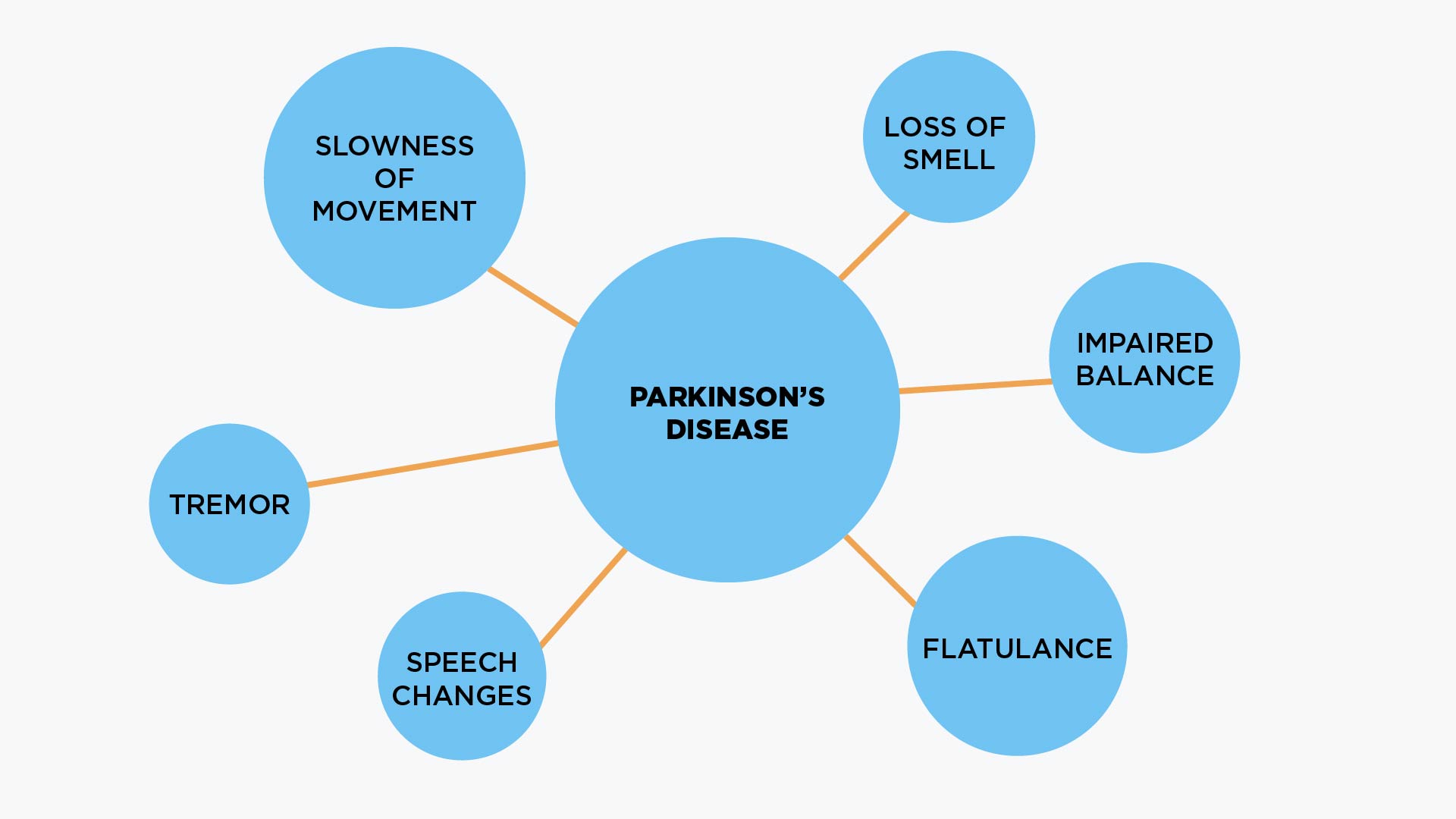
Parkinson’s Disease (PD) is a medical condition that affects functional mobility through stiffness of the body, immobility, and difficulty in initiating actions. It is the second most common neurodegenerative disease, and it is characterised by both physical manifestations as well as non-motor problems (e.g. psychological, social).
Despite the variety of treatment options, disease progression usually leads to impairments at different levels of body function, limitations in a wide variety of activities of daily living (ADLs), and in severe disability and increasing dependence. Gradually, it reduces health-related quality of life (HrQoL) and increases the burden of patients and caregivers. Besides medications, a number of non-drug strategies and therapies can be helpful in alleviating the disease burden.

Osteoarthritis (OA) is the most common joint disorder, typically affecting weight-bearing joints (knees and hips, ankles and feet) and the spine. In OA, the effects of ageing, wear and tear, previous damage, or other diseases that have secondary effects on the joints, cause damage to the cartilage and bone in and around joints, leading to symptoms of pain, stiffness, immobility and deformity.
Causes of OA include genetic predisposition, poor alignment of joints, overuse and injury, increased physical stress, and other joint diseases. Management options include physiotherapy, supports, lifestyle modification and weight loss, medications, joint injections, and various types of surgery.
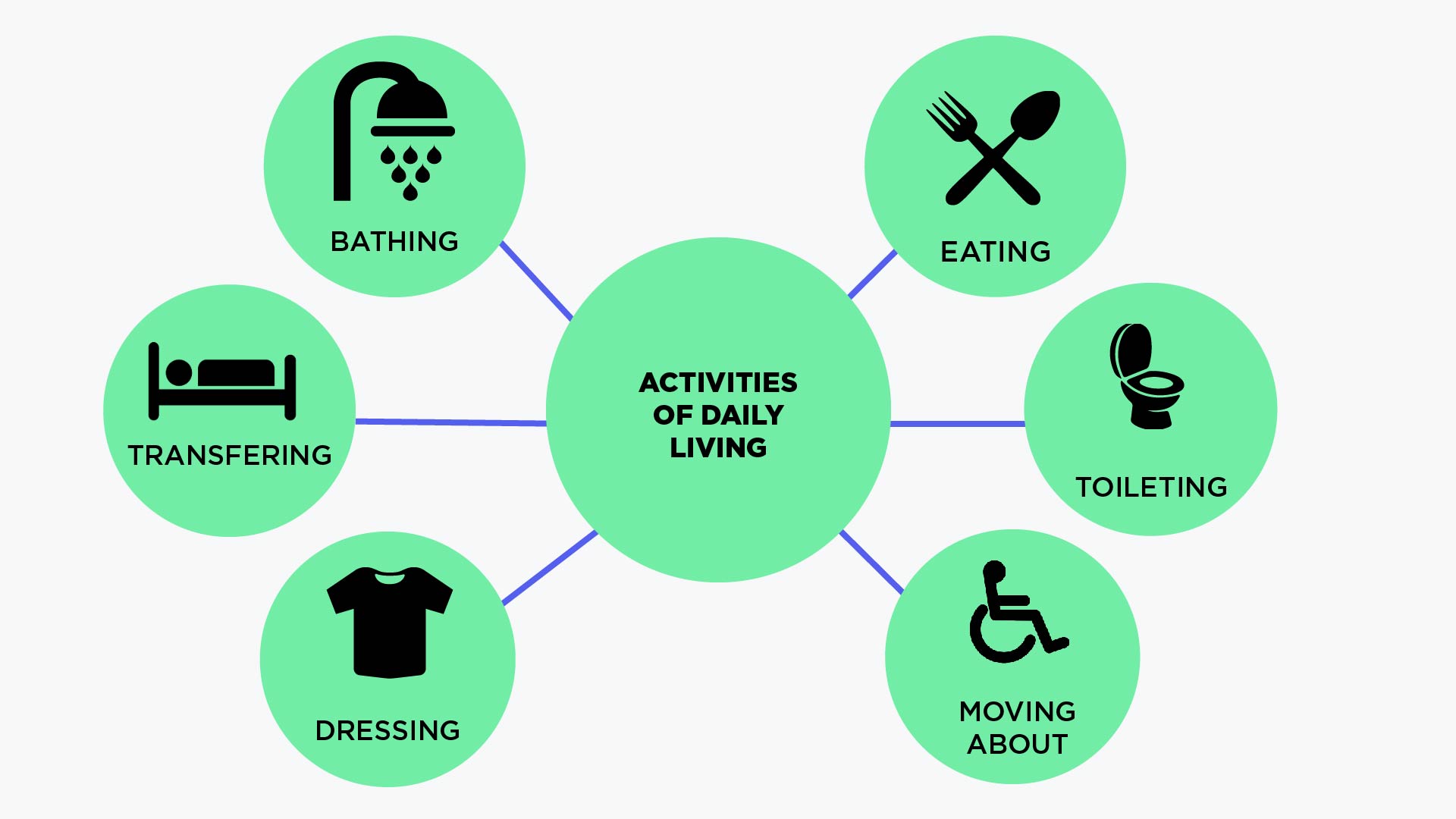
Functional mobility and the activities of daily living (ADLs) are closely related and intertwined. Common ADLs include fundamental and crucial activities such as dressing/bathing, eating, ambulating (walking), movement and transferring, toileting, and hygiene.
Functional Mobility, defined as the physiological ability of people to move independently and safely in a variety of environments in order to accomplish functional activities or tasks and to participate in ADLs at home, at work and in the community, is increasingly used as a measurable health outcome in research studies and practical projects, and as a global and ecological evaluation of patients' health status.
Maintaining ADLs plays a crucial role in promoting general health and facilitating healthy physical and mental function at home and in the community. Conversely, impaired functional mobility and ADLs have been found to be associated with greater risk of falls, loss of independence and need for institutional care.